


Study with the several resources on Docsity

Earn points by helping other students or get them with a premium plan


Prepare for your exams
Study with the several resources on Docsity

Earn points to download
Earn points by helping other students or get them with a premium plan
Community
Ask the community for help and clear up your study doubts
Discover the best universities in your country according to Docsity users
Free resources
Download our free guides on studying techniques, anxiety management strategies, and thesis advice from Docsity tutors
It can be utilized for serial assessment of patients to track response to therapy. Appearance: The “Tickles” (TICLS) Mnemonic. Characteristic. Normal features.
Typology: Study notes
1 / 2

This page cannot be seen from the preview
Don't miss anything!

This reference card should not be considered to replace or supercede regional prehospital medical treatment protocols.
Supported in part by project grant #6 H33 MC 00036 from the Emergency Services for Children program, HRSA, USDHHS in cooperation with NHTSA Rev. 1/
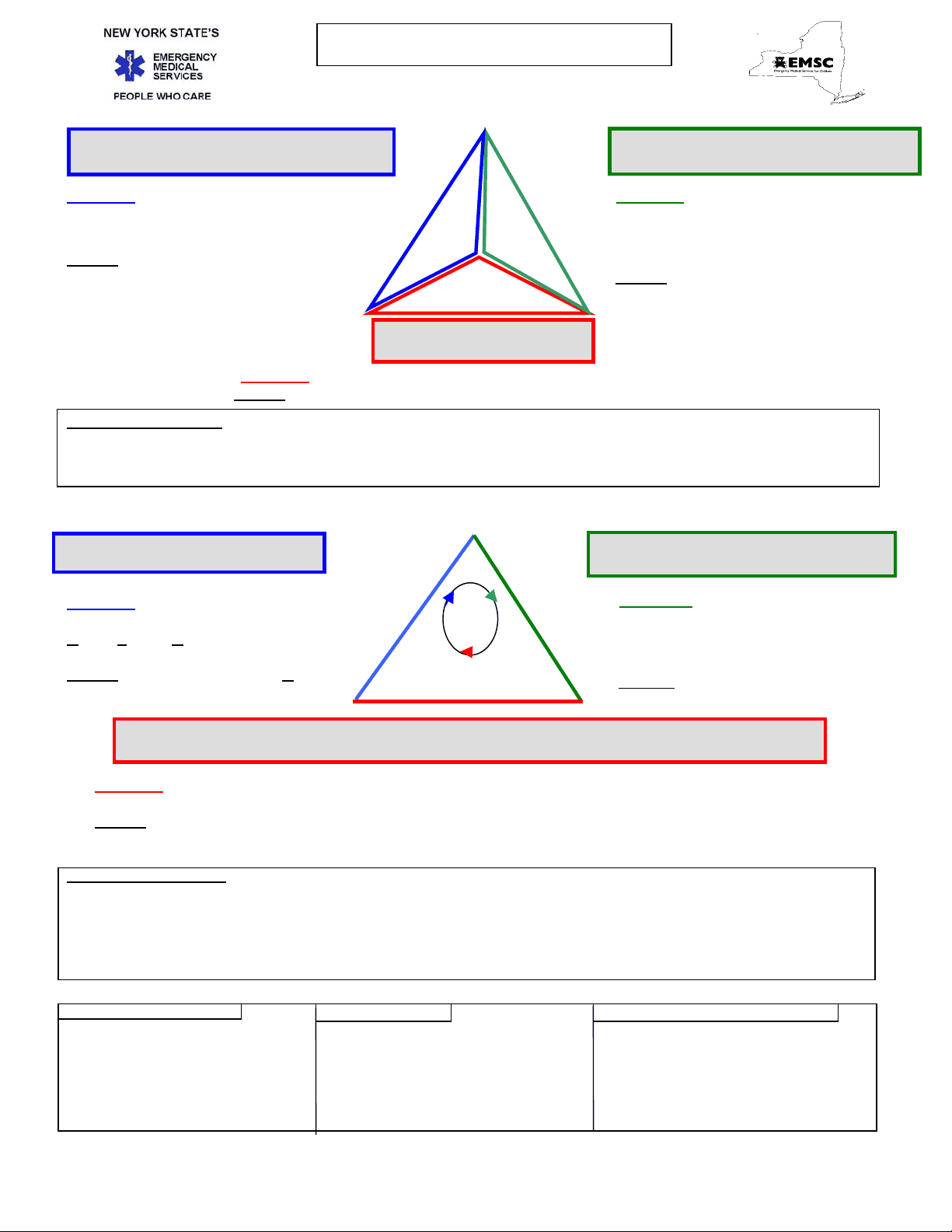
(First view of patient)
Abnormal : Abnormal or absent cry or speech. Decreased response to parents or environmental stimuli. Floppy or rigid muscle tone or not moving. A B
Normal : Normal cry or speech. Responds to parents or to environmental stimuli such as lights, keys, or toys. Good muscle tone. C Moves extremities well.
Abnormal : Increased/excessive (nasal flaring, retractions or abdominal muscle use) or decreased/absent respiratory effort or noisy breathing.
Normal : Breathing appears regular without excessive respiratory muscle effort or audible respiratory sounds.
Abnormal : Cyanosis, mottling, paleness/pallor or obvious significant bleeding. Normal : Color appears normal for racial group of child. No significant bleeding.
Decision/Action Points:
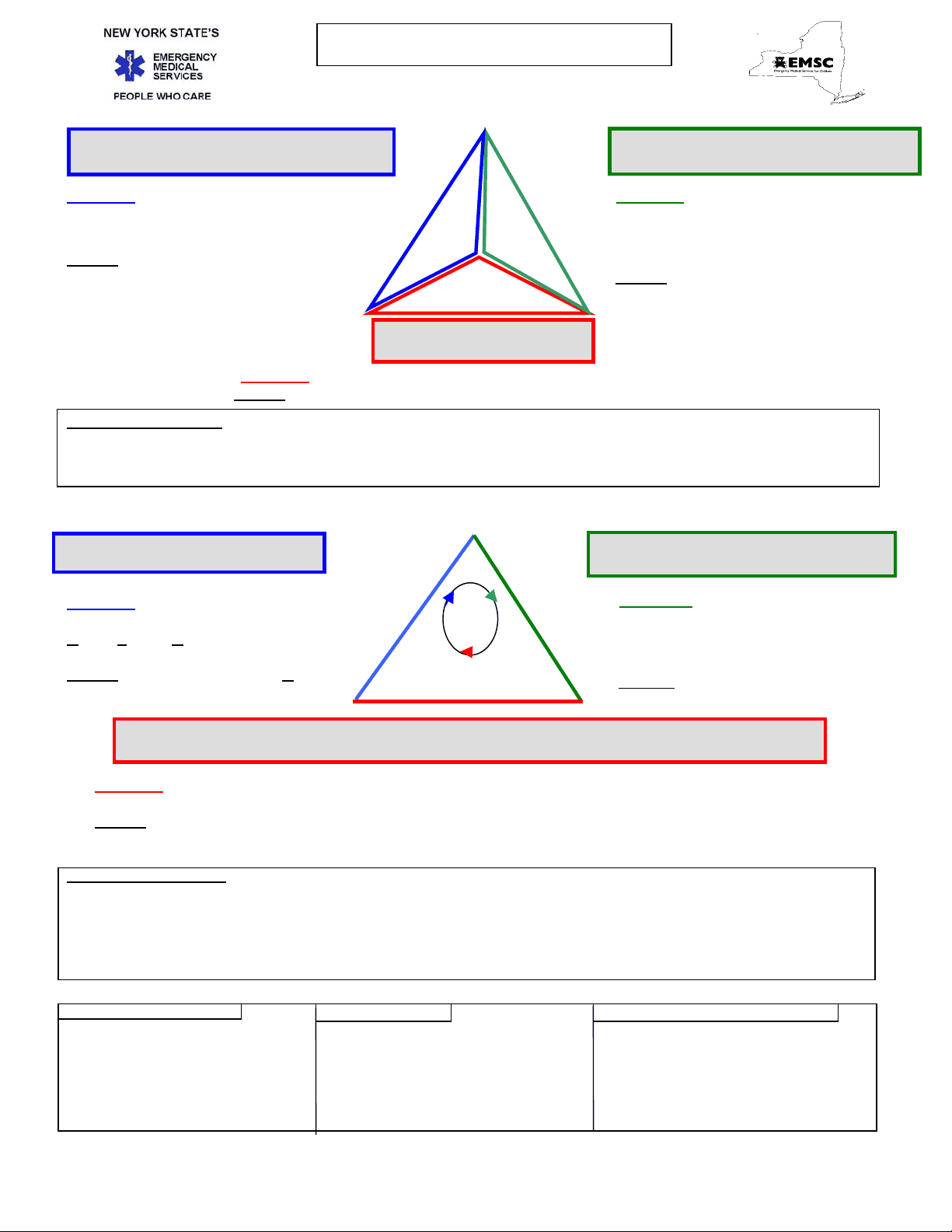
(Primary Survey)
Abnormal : Obstruction to airflow. Gurgling, stridor or noisy breathing. V erbal , P ain , or U nresponsive on AVPU scale.
Normal : Clear and maintainable. A lert on Continue assessment AVPU scale. throughout transport
Abnormal: Presence of retractions, nasal flaring, stridor, wheezes, grunting, gasping or gurgling. Respiratory rate outside normal range. Central cyanosis.
Normal: Easy, quiet respirations. Respiratory rate within normal range. No central cyanosis.
Abnormal : Cyanosis, mottling, or pallor. Absent or weak peripheral or central pulses; Pulse or systolic BP outside normal range; Capillary refill > 2 sec with other abnormal findings. Normal : Color normal. Capillary refill at palms, soles, forehead or central body ≤ 2 sec. Strong peripheral and central pulses with regular rhythm.
Decision/ Action Points:
Normal Respiratory Rate: Normal Pulse Rate: Lower Limit of Normal Systolic BP: Infant (<1yr): 30- 60 Infant: 100-160 Infant: >60 (or strong pulses) Toddler (1-3yr): 24 -40 Toddler: 90-150 Toddler: >70 (or strong pulses) Preschooler(4-5yr): 22- 34 Preschooler: 80-140 Preschooler: > School-age(6-12yr): 18 -30 School-age: 70-120 School-age: > Adolescent(13-18yr): 12 -20 Adolescent: 60-100 .Adolescent: > Pulses slower in sleeping child / athlete Estimated min.SBP >70 + (2 x age in yr)
This reference card should not be considered to replace or supercede regional prehospital medical treatment protocols. Supported in part by project grant #6 H33 MC 00036 from the Emergency Services for Children program, HRSA, USDHHS in cooperation with NHTSA Rev. 1/
Critical Absent airway, breathing or circulation (cardiac or respiratory arrest or severe traumatic injury)
Unstable Compromised airway, breathing or circulation (unresponsive, respiratory distress, active bleeding, shock, active seizure, significant injury, shock, near-drowning, etc.)
Potentially Normal airway, breathing & circulation Unstable but significant mechanism of injury or illness (post-seizure, minor fractures, infant < 3mo with fever, etc.)
Stable Normal airway, breathing & circulation No significant mechanism of injury or illness (small lacerations or abrasions, infant ≥ 3mo with fever)
Dry, Warm, Position, Tactile Stimulation. Suction Mouth then Nose. Call for ALS back-up. Administer O2 as needed.
Apnea/Gasping, HR <100 or central cyanosis
Ventilate with BVM @ 40-60/min
HR<60 after 30 sec BVM Chest Compressions @ 120/min - 3: 1/3 to 1/2 chest depth 2 thumb encircle chest or 2 fingers
ALS available & HR <
Epinephrine 0.01-0.03mg/kg 0 pts 1 pt 2 pts IV/IO/ET Pulse Absent <100 ≥ 100 1:10,000 Resp Absent Slow Good q 3-5 min Irregular Tone Limp Some Active flexion motion Reflex None Grimace Cough Sneeze Color Blue Pink Body All Blue Limbs Pink
Asystole or PEA
Assess airway & start CPR Intubate & ventilate with oxygen
Epinephrine: 0.01 mg/kg 1:10,000 IV/ IO 0.1 mg/kg 1:1000 ET .Continue Epinephrine q 3-5 min, same dose Consider hi dose 0.1 mg/kg 1:1000 IV/IO/ET
Consider possibility of hypoxia, hypovolemia, hypothermia, hyper/hypokalemia, tamponade, tension .pneumothorax, toxins/poisons/drugs or .thromboembolism & treat if present.
Infants Children /Adults
Spontaneous 4 Spontaneous To speech/sound 3 To speech To pain 2 To pain No response 1 No response Verbal Response Coos or babbles 5 Oriented Irritable crying 4 Confused Cries to pain 3 Inappropriate words Moans to pain 2 Incomprehensible None 1 None Motor Response Spontaneous .6 Obeys commands Withdraws touch 5 Localizes pain Withdraws pain .4 Withdraws pain Abnormal flexion 3 Abnormal flexion Abnormal extension 2 Abnormal extension No response 1 No response
Infant Child Teen <1yr 1-8yr 9-18yr
Ventilation only 20/min 20/min 12/min
CPR method 2 fingers 1 hand 2 hand
Chest Depth 1/3-1/2 1/3-1/2 1/3-1/
Compression Rate ≥ 100/min 100/min 100/min
Ratio 5:1 5:1 5:
CPR should be started for HR<60. Only AEDs with pediatric capabilities should be used on patients < 8 yrs. of age (approx. 25kg or 55lb).
VF or pulseless VT Defibrillate up to 3 times as needed 2j /kg 4j /kg 4j /kg Start CPR, intubate, ventilate with O 2
Epinephrine: 0.01 mg/kg 1:10,000 IV/ IO 0.1 mg/kg 1:1000 ET Defibrillate 4j / kg Amiodarone 5mg/kg IV/IO or Lidocaine 1mg / kg IV/ IO/ ET or Magnesium 25-50mg/kg IV/ IO (for torsades de pointes or hypomagnesemia) Defibrillate 4j / kg
Bradycardia
Assess airway & give oxygen
Intubate if decreased consciousness Start CPR if HR<60.
Epinephrine: 0.01 mg/kg 1:10,000 IV/ IO 0.1 mg/kg 1:1000 ET Continue Epinephrine q 3-5 min, same dose
Atropine 0.02 mg/kg IV/ IO / ET minimum dose 0.1 mg maximum dose 0.5 mg child; 1.0 mg teen