


Study with the several resources on Docsity

Earn points by helping other students or get them with a premium plan


Prepare for your exams
Study with the several resources on Docsity

Earn points to download
Earn points by helping other students or get them with a premium plan
Community
Ask the community for help and clear up your study doubts
Discover the best universities in your country according to Docsity users
Free resources
Download our free guides on studying techniques, anxiety management strategies, and thesis advice from Docsity tutors
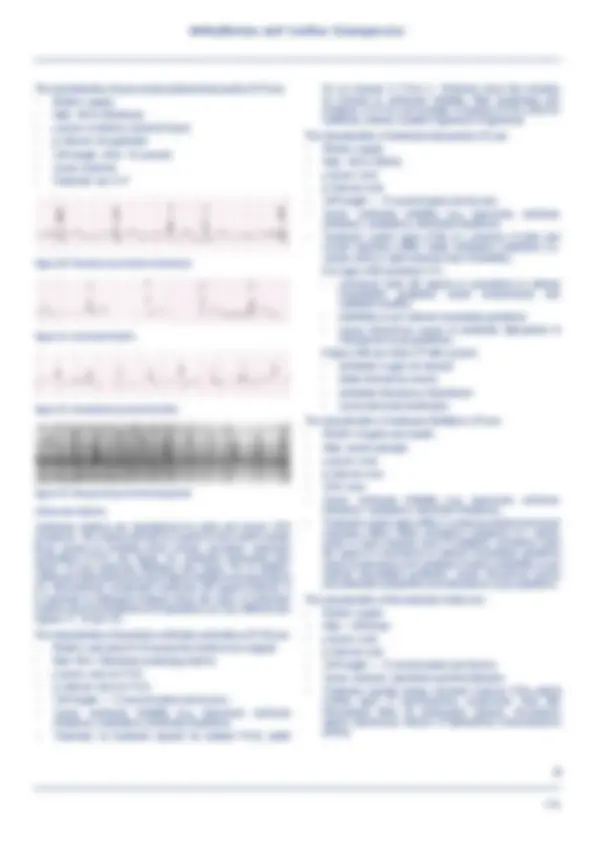
perfect rhythm; which is referred to as normal sinus rhythm (see ... The characteristics of premature junctional contraction (PJC) are: •. Rhythm: early ...
Typology: Lecture notes
1 / 7

This page cannot be seen from the preview
Don't miss anything!

Sandra Goldsworthy, David Waters
After completing this chapter you will be able to:
general rule, when a patient’s heart rate is less than 60/minute critical care nurses should be prepared to immediately assess for signs of decreased cardiac output (i.e. decreased level of consciousness, hypotension, chest pain). The characteristics of sinus bradycardia are:
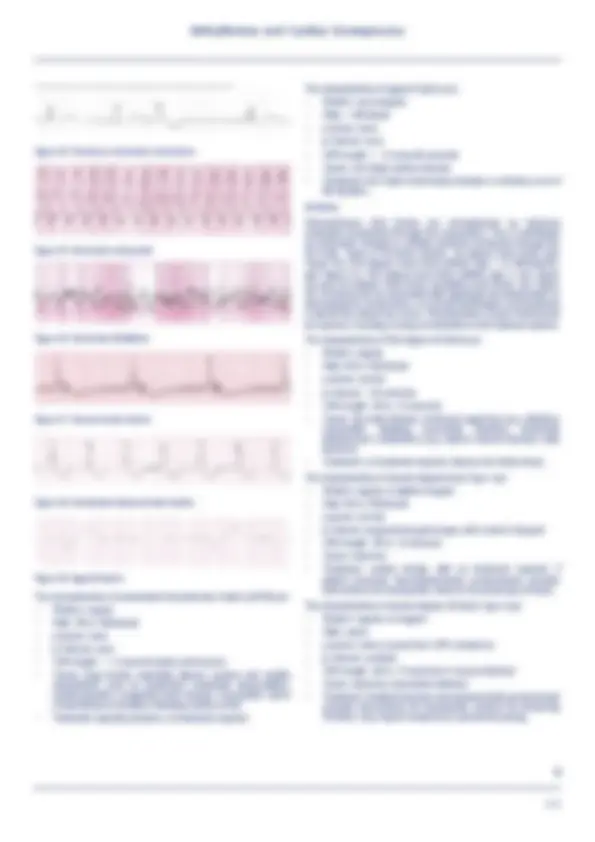
The characteristics of paroxysmal junctional tachycardia (PJT) are:
Figure 14. Premature ventricular contractions Figure 15. Ventricular tachycardia Figure 16. Ventricular fibrillation Figure 17. Idioventricular rhythm Figure 18. Accelerated idioventricular rhythm Figure 19. Agonal rhythm The characteristics of accelerated idioventricular rhythm (AIVR) are:
Answers
Aehlert B (2018). ECGs Made Easy, 6th ed. Mosby: St. Louis, Missouri. Link M, Berkow L, Kudenchuk P et al. (2015). Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care, Part 7: Adult Advanced Cardiac Life Support. Circulation 132(18 Suppl 2): S444-64. Goldsworthy S (2012). Coronary Care 1 and 2 Manual. Durham College Continuing Education: Oshawa, Canada. Walraven G (2011). Basic Arrhythmias 7th ed. Pearson Publishers: Toronto, Ontario. Other helpful resources ECGlibrary.com. [for practice]. Available at: https://ecglibrary.com/ ecghome.php.